Keratoconus causes, symptoms and 10 treatments
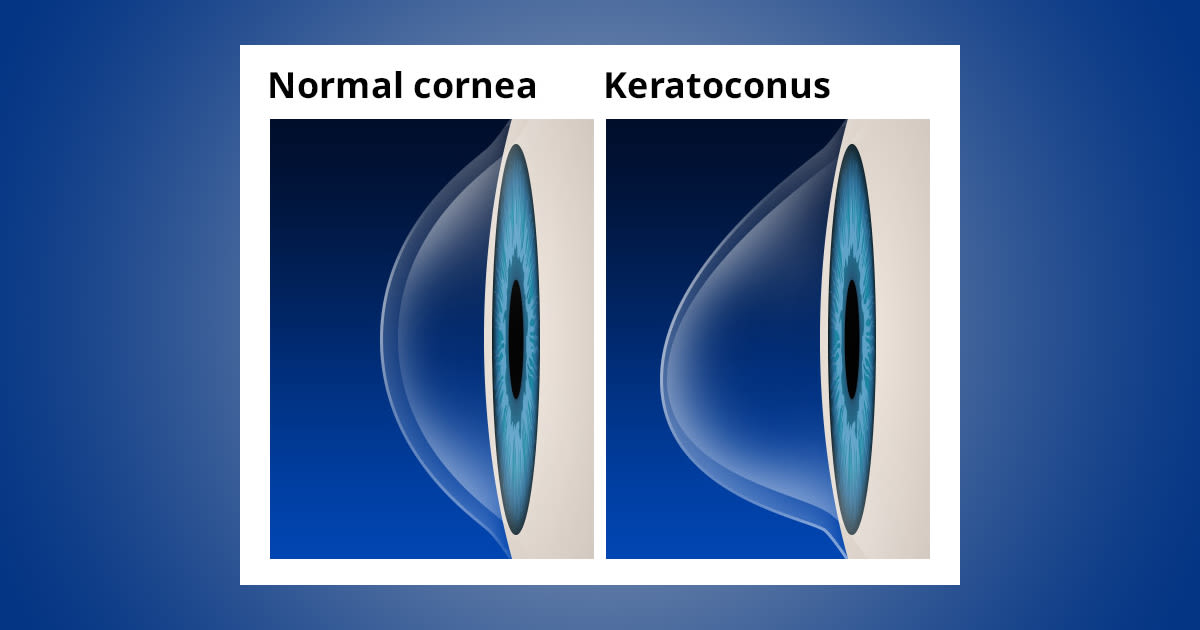
Keratoconus is a progressive eye disease that causes a thinning of the clear front surface of the eye (cornea) and distorts the cornea into a cone-like shape.
Keratoconus causes distorted vision that cannot be corrected with spectacles.
Most cases of keratoconus become apparent during a person's teens or early 20's. It can affect one or both eyes.
Keratoconus symptoms and signs
As the cornea becomes more irregular in shape, it causes progressive short sightedness and irregular astigmatism to develop, creating additional problems with distorted and blurred vision.
Glare and light sensitivity also commonly occur with keratoconus.
A person with keratoconus often experiences changes in their eyeglass prescription every time they visit their eye doctor.
What causes keratoconus?
New research suggests the weakening of the corneal tissue that leads to keratoconus may be due to an imbalance of enzymes within the cornea. This imbalance makes the cornea more susceptible to oxidative damage from compounds called free radicals, causing it to weaken and bulge forward.
Risk factors for oxidative damage and weakening of the cornea include a genetic predisposition, explaining why keratoconus often affects more than one member of the same family.
Keratoconus also is associated with overexposure to ultraviolet rays from the sun, excessive eye rubbing, a history of poorly fitted contact lenses and chronic eye irritation.
Keratoconus treatment
In the mildest form of keratoconus, eyeglasses or soft contact lenses may help. But as the disease progresses and the cornea thins and becomes increasingly more irregular in shape, glasses and regular soft contact lens designs no longer provide adequate vision correction.
Treatments for progressive keratoconus include:
1. Corneal crosslinking
This procedure, also called corneal collagen cross-linking or CXL, strengthens corneal tissue to halt bulging of the eye's surface in keratoconus.
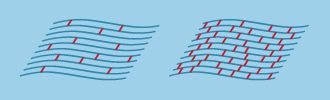
The aim of corneal cross-linking is to strengthen the cornea by increasing the number of "anchors" that bond collagen fibres together. (Diagram: Boxer Wachler Vision Institute)
There are two versions of corneal crosslinking: epithelium-off and epithelium-on.
With epithelium-off crosslinking, the outer layer of the cornea (called the epithelium) is removed to allow entry of riboflavin, a type of B vitamin, into the cornea, which then is activated with UV light.
With the epithelium-on method (also called transepithelial crosslinking), the corneal epithelium is left intact during the treatment. The epithelium-on method requires more time for the riboflavin to penetrate into the cornea, but potential advantages include less risk of infection, less discomfort and faster visual recovery, according to supporters of this technique.
Corneal crosslinking may reduce significantly the need for corneal transplants among keratoconus patients. It also is being investigated as a way to treat or prevent complications following LASIK or other vision correction surgery.
Using a combination of corneal crosslinking and Intacs implants also has demonstrated promising results for treating keratoconus. Also, progressive mild to moderate keratoconus has been safely and successfully treated with a combination of corneal crosslinking and implantation of a toric phakic IOL.
2. Custom soft contact lenses
Recently, contact lens manufacturers have introduced custom soft contact lenses specially designed to correct mild-to-moderate keratoconus.
These lenses are made-to-order based on detailed measurements of the person's keratoconic eye(s) and may be more comfortable than gas permeable lenses (GPs) or hybrid contact lenses for some wearers.
Custom soft contact lenses are available in a very wide range of fitting parameters for a customised fit and are larger in diameter than regular soft lenses for greater stability on a keratoconic eye.
In a recent study of the visual performance of toric soft contacts and rigid gas permeable lenses for the correction of mild keratoconus, though GP lenses provided better visual acuity in low-contrast situations, soft toric lenses performed equally well in high-contrast acuity testing.
3. Gas permeable contact lenses
If spectacles or soft contact lenses cannot control keratoconus, then gas permeable contact lenses usually are the preferred treatment. GP lenses vault over the cornea, replacing its irregular shape with a smooth, uniform refracting surface to improve vision.
Fitting contact lenses on an eye with keratoconus often is challenging and time-consuming. You can expect frequent return visits to your optician so he or she can fine-tune the fit and your prescription, especially if your keratoconus continues to progress.
4. "Piggybacking" contact lenses
Because fitting a gas permeable contact lens over a cone-shaped cornea can sometimes be uncomfortable for a person with keratoconus, some eye doctors advocate "piggybacking" two different types of contact lenses on the same eye.
For keratoconus, this method involves placing a soft contact lens, such as one made of silicone hydrogel, over the eye and then fitting a GP lens over the soft lens. This approach increases wearer comfort because the soft lens acts like a cushioning pad under the rigid GP lens.
Your optician will monitor closely the fitting of "piggyback" contact lenses to make sure enough oxygen reaches the surface of your eye, which can be a problem when two lenses are worn on the same eye. However, most modern contacts — both GP and soft — typically have adequate oxygen permeability for a safe "piggyback" fit.
5. Hybrid contact lenses
Hybrid contact lenses combine a highly oxygen-permeable rigid centre with a soft peripheral "skirt." These lenses were designed specifically for keratoconus, and the central GP zone of the lens vaults over the cone-shaped cornea for increased comfort.
Hybrid contact lenses provide the crisp optics of a gas permeable contact lens and wearing comfort that rivals that of soft lenses. They are available in a wide variety of parameters to provide a fit that conforms well to the irregular shape of a keratoconic eye.
6. Scleral and semi-scleral lenses
These are large-diameter gas permeable contacts — large enough that the periphery and edge of the lens rest on the "white" of the eye (sclera).
Scleral lenses cover a larger portion of the sclera, whereas semi-scleral lenses cover a smaller area.
Because the centre of scleral and semi-scleral lenses vaults over the irregularly shaped cornea, these lenses don't apply pressure to the eye's cone-shaped surface for a more comfortable fit.
Scleral lenses also are more stable than conventional gas permeable contact lenses, which move with each blink because they cover only a portion of the cornea.
7. Prosthetic lenses
Because keratoconic eyes are so challenging to fit, patients with severe disease often require an advanced scleral lens design that doubles as a prosthetic shell.
These custom lenses are made with advanced imaging technology to enable the back surface of the lens to match the unique irregularities of keratoconic eyes.
Because of the precise nature of the back-surface fit, high quality and individualised optics can be placed on the front surface of the device.
Fitting custom prosthetic lenses for keratoconus requires special technology and fitting expertise and may not be available in some areas.
8. Intacs
Intacs (Addition Technology) are clear, arc-shaped corneal inserts that are surgically positioned within the peripheral cornea to reshape the front surface of the eye for clearer vision.
Intacs may be needed when a person with keratoconus no longer can obtain functional vision with contact lenses or spectacles.
Several studies show that Intacs can improve the best spectacle-corrected visual acuity (BSCVA) of a keratoconic eye by an average of two lines on a standard eye chart.
The implants also have the advantage of being removable and exchangeable. The surgical procedure takes only about 10 minutes.
9. Topography-guided conductive keratoplasty
Topography-guided conductive keratoplasty (CK) is a procedure that uses a hand-held tool to deliver energy from radio waves to specific points in the periphery of the cornea to reshape the eye's front surface.
A topographic "map" created by computer imaging of the eye's surface helps create individualised treatment plans.
Though not as popular as other treatment options, topography-guided CK may be helpful to reduce irregular astigmatism caused by keratoconus.
10. Corneal transplant
In some cases of advanced keratoconus, the only viable treatment option is a cornea transplant, also called a penetrating keratoplasty (PK or PKP). It can take several months for your vision to stabilise after a cornea transplant, and it’s likely you will need spectacles or contact lenses afterwards to see clearly.
Also, there is the risk of infection and graft rejection after a transplant procedure.
For these and other reasons, a cornea transplant typically is recommended only if no other keratoconus treatments are successful.
NEED AN EYE TEST? Find an optician near you and schedule an appointment.
Page published on Thursday, 27 June 2019






