Cataract surgery complications
Millions of people successfully undergo cataract surgery every year, and cataract surgery complications are relatively rare.
Potential cataract surgery complications include:
Posterior capsule opacity (PCO)
Intraocular lens dislocation
Eye inflammation
Light sensitivity
Photopsia (perceived flashes of light)
Macular edema (swelling of the central retina)
Ptosis (droopy eyelid)
Ocular hypertension (elevated eye pressure)
When cataract surgery complications do occur, most are minor and can be successfully treated medically or with additional surgery.
Posterior capsule opacity
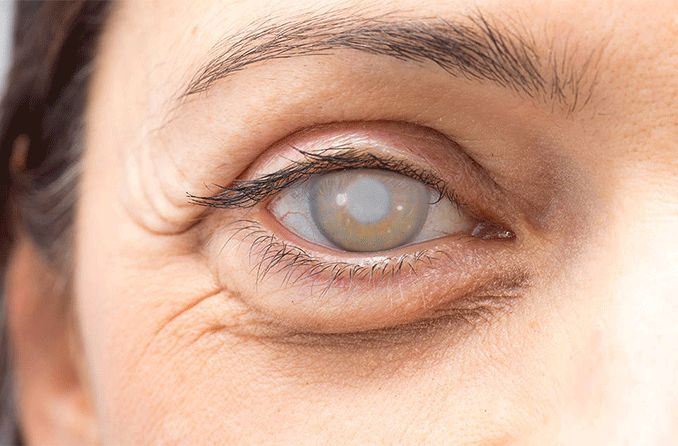
One of the most common cataract surgery complications is a posterior capsule opacity (also called posterior capsule opacification or PCO).
Although some people call PCO a "secondary cataract," it really is not a cataract. Once a cataract is removed, it does not come back.
In cataract surgery, your surgeon removes the cloudy natural lens of your eye (cataract) and replace it with an intraocular lens (IOL).
During this procedure, much of the thin clear membrane that surrounds the natural lens (called the lens capsule) is intentionally left intact.
In most cases, the lens capsule remains clear after cataract surgery. In some cases, however, the posterior portion of the capsule (the part left intact) becomes hazy. This posterior capsule opacification can occur during cataract surgery recovery or even months later.
Treating posterior capsule opacification
Fortunately, PCO can be effectively treated with a procedure called a YAG laser capsulotomy. During the procedure, a hole is created in the central zone of the cloudy capsule and vision is quickly restored.
There are three steps to a YAG laser capsulotomy:
Eye drops are used to dilate the pupil. This enables your eye doctor to see the entire lens capsule.
The laser removes the hazy posterior capsule from your line of sight without making an incision or touching the eye.
Medicated eye drops are applied after the procedure to prevent inflammation.
The procedure takes only a few minutes and is painless.
Following a YAG laser capsulotomy, you may resume normal activities immediately. You may experience some floaters afterward. These usually resolve within a few weeks.
Most people can expect their vision to improve within a day. Consult your eye doctor immediately if your vision worsens or fails to improve after a laser capsulotomy.
Because the YAG laser removes the central zone of the cloudy posterior capsule behind the intraocular lens, the condition cannot return. So only one laser treatment is required to permanently eliminate vision loss caused by PCO after cataract surgery.
YAG laser capsulotomy risks
Complications from a YAG laser capsulotomy are rare. However, the procedure can increase risk of retinal detachment to some degree.
Research suggests the lifetime risk of a detached retina as a cataract surgery complication is about 1 percent. That risk increases to about 2 percent if cataract surgery is followed by a YAG laser capsulotomy.
Dislocated IOL
Another potential cataract surgery complication is a dislocated intraocular lens (IOL). This can cause vision problems, including double vision.
IOL dislocations are rare, but should one occur, your cataract surgeon usually can reposition it surgically. In some cases, the implant must then be sewn in place to secure it, or it may be removed and replaced with a different IOL.
Other cataract surgery complications
Other potential cataract surgery complications range from inflammation to devastating vision loss. The risk of severe vision loss is very rare and may occur as a result of infection or bleeding inside the eye.
Some cataract surgery complications occur a long time after the procedure. For example, a detached retina can occur months or years after a perfectly successful cataract procedure. If you suddenly begin seeing floaters or flashes of light (symptoms of retinal detachment) at any time after cataract surgery, consult your eye doctor immediately.
Other potential cataract surgery complications include:
Increased pressure in the eye (ocular hypertension).
Droopy eyelid (ptosis).
If you notice these or other unusual symptoms after cataract surgery, consult your eye doctor for evaluation and treatment.
Vision problems after cataract surgery
If you have any problem with sensitivity to sunlight after cataract surgery, eyeglasses with photochromic lenses, which darken automatically to UV rays, often can provide relief.
Also, for residual refractive error and presbyopia after surgery, progressive lenses with anti-reflective coating often can sharpen your vision for activities like night driving and reading.
People whose vision fails to improve after cataract surgery often have underlying eye disorders, such as age-related macular degeneration, diabetic retinopathy and other eye conditions.
Routine eye exams remain very important after cataract surgery to monitor the health of your eyes and the clarity of your vision.
Page published on Friday, January 3, 2020